
Finding, training and retaining staff is the single most pressing issue facing NHS Scotland as the pandemic prompts an exodus from the frontline, experts warn today.
A range of specialists say a crippling shortage of staff is the most fundamental and threatening issue facing the service.
Official figures show more than half of consultant vacancies are open for more than six months and a third of nursing vacancies are open for more than three months.
Meanwhile, 5,500 doctors applied to work overseas last year, up on 2020 despite the uncertainty of the pandemic.
The Scottish Government published a workforce plan to deal with a recruitment crisis in 2019 but Brexit and the pandemic has since intensified the problem.
A new report about the state of the NHS will be released by Scotland’s spending watchdog, the Auditor General for Scotland Stephen Boyle, next month and it is expected to be critical of progress.
Boyle said: “We have been saying for a number of years that the NHS in Scotland is not financially sustainable under its current model. The pandemic has turned the notch up on those pressures. Health boards are facing as much financial uncertainty as ever, and many services remain under severe strain.
“The Scottish Government has ambitious workforce plans but what we also know is that the NHS has historically struggled to recruit enough workers with the right skills, so a real challenge remains there.”

The struggle to recruit, train and retain staff is the single most pressing issue facing NHS Scotland, according to Dr Jillian Evans, head of NHS Grampian’s Health Intelligence Unit.
She said: “There is a continuing, enduring, number of vacancies and gaps, and challenges in getting highly skilled people into posts.
“I don’t think the way the NHS is and has been working over the last several decades is sustainable for the future.
“It is very pressurised. I don’t know anyone who sticks to a normal working week. I don’t know what a normal working week is anymore. Everybody has to go over and above. It’s the enduring nature of having to do more and more and more and I think people are evaluating what’s important to them in their lives. I think that’s why it’s difficult to attract people in.
“There aren’t enough doctors coming through, there aren’t enough nurses. But you’ve got to create the right working conditions for people to get a sense of fulfilment and that’s what is difficult at the moment.”
Doctors’ leaders fear NHS Scotland staff are facing unprecedented pressure due to workforce shortages as new figures reveal more than 5,500 UK doctors last year applied for references to work overseas.
In 2020 the numbers of doctors applying to work overseas fell to 5,152 but despite the ongoing pandemic and strict quarantine measures operated by other countries, the number climbed to 5,576 last year with more expected.
The figures were released by the General Medical Council, which must grant certificates of current professional status before doctors can work abroad.
Long waits for Scots seeking vital help from lifeline NHS 24 service
Andrew Goddard, president of the Royal College of Physicians, said: “Workforce is the key limiting factor in providing safe urgent and emergency care services and bringing down the huge backlogs caused by Covid. Even before the pandemic, half of consultant vacancies went unfilled – the pressure NHS staff are now facing is unprecedented.
“With more staff deciding to work abroad, there is yet more urgency for the government to put in place proper workforce planning to ensure we are training enough doctors now to meet future demand. There must also be urgent action to maximise retention of the staff we currently have.”
Last week the Royal College of Physicians reported that more than two thirds of doctors (69%) have felt overwhelmed at work at least once in the past three weeks and the BMA’s concern was echoed by campaign group Doctors Association UK (DAUK), who describe staff shortages as the biggest crisis the NHS faces.
“This figure of over 5,500 is unsurprising given the current conditions for staff working in the NHS, where even basics such as fully staffed rotas, breaks and annual leave are a struggle to achieve. Staffing is the biggest crisis facing the NHS right now and DAUK are campaigning towards solutions for this.
“We could learn a lot from our overseas colleagues on how to care for healthcare workers and maintain a happy work-life balance.”
Not enough doctors or nurses are being trained to replace those leaving or retiring, according to Mark Dayan, policy analyst at the Nuffield Trust, an independent think tank set up in 1939.
He said: “The workforce in Scotland has not been growing at a rate that will keep up with demand.
“There is a vicious circle where the NHS is a difficult place to work and, because staffing numbers are so low, it encourages people to seek alternatives.
“In general the UK has quite a big gap between nursing and medical pay, compared to what you see in other countries. Australia and North America are paying far more.
“So, I do think the UK faces a structural problem in that it’s English-speaking and many of the other English speaking countries are among the highest paying in the world.
“Given that, and the shortfall in training, it’s not surprising that we are where we are.”
One short-term solution to the recruitment crisis is to allow fresh waves of migration, according to Dayan.
He said: “We need to set the workforce on a more secure path by improving recruitment and retention. A big part of that is international recruitment. Post-Brexit there was a big drop off in EU migration which is a serious problem because that was a major contributor to the nursing workforce in particular.
“In the last few years the UK has actually been quite successful in getting recruitment back on line from countries like the Philippines. For Scotland, the big question is how we get those people here.”
A recent Lancet report on the future of the NHS said the UK has fewer nurses and doctors per person than most other high-income countries. The May 2021 report said NHS workforce planning in the UK is ineffective and has consistently failed to respond to persistent shortfalls in staffing.
The report said Scotland has made progress in workforce planning but must also prioritise the health, morale and wellbeing of the current workforce to maximise recruitment and retention of staff.
Co-author of the report, professor Aziz Sheikh OBE, director of the Usher Institute at the University of Edinburgh, said: “Morale and burnout in the workforce is a big-ticket issue.
“The sixth wealthiest nation in the world should be able to achieve almost anything, really. Clearly the pandemic has had a considerable impact on public finances and my view is Brexit probably has too.
“That makes this more difficult but at some point the bull has to be grabbed by the horn. Otherwise, this has all sorts of other implications for society.”
It is not just about salaries. We need to do more for staff
– Derek Bell
by Janet Boyle
The need for the NHS to train and retain skilled, committed staff has never been more pressing, according to one of its most experienced, influential doctors.
There are few more qualified to assess the threats to the health service as Derek Bell, the first UK professor of acute medicine, author of more than 200 research papers and the lead on a series of national policy initiatives.
Stepping back from the frontline after 42 years, Bell, a former president of the Royal College of Physicians of Edinburgh, sees risks and opportunities in the years ahead but keeping skilled staff is paramount, particularly as the stress of dealing with the pandemic takes a toll.
He said: “We need to ensure we have the number of staff needed to meet the demands of the service. Recruitment and retention are key and it is not all about salary. Have we, for example, created a good working environment, good rest areas adequate facilities for food and drink?
“We must actively consider co-locating or returning to sports and leisure facilities on site. These should not be seen as luxuries, but necessities, along with opportunities to develop and build careers. We should encourage every member of staff to contribute to improving services, a bottom-up rather than top-down approach.”
Bell was a member of the independent working group looking at the exhausting working week of many junior doctors: “The challenge we face is although numbers of posts have increased the intensity of work and work-life balance has changed hugely and at any one time we have to employ locums to fill the gaps.
“We have to increase the number of students training in medical and aligned careers and ensure we have excellent retention processes in place.”
He believes the NHS should be rigorous in seeking to improve services and ruthless if reforms are not working.
He said: “We should also be willing to learn from all health care systems – Scandinavia, Netherlands, Australia and developing countries – which often show innovation leaps such as use of mobile health.”
Mobile health includes the use of mobile phones and other wireless technology in medical care.
Long distance monitoring of heart patients on the Western Isles through regular cardiac readings sent down the phone line is one example but it also includes surveillance for diseases, treatment and, vitally, epidemic outbreak tracking as well as treating patients with chronic diseases.
Bell, 66, who grew up in a tenement in Dundee’s North Street, has enjoyed an illustrious career since becoming the first in his family to go to university, armed with a stethoscope his granny bought him for his first year as a medical student in Edinburgh.
He worked in the capital in respiratory and general medicine before moving into ICU and then onto acute medicine.
There, he became associate medical director before moving to his professorship at Imperial College London in London.
Until Christmas he was still doing a 10- to 12-hour day on an on-call rota: “I worked a three to four-day week at my hospital Chelsea and Westminster, London, on a one-in-eight on-call rota, mainly weekends.”
He has been enlisted on a number of national policy initiatives including the development of the successful National Early Warning Score (NEWS) to support standardisation of patient care across the UK and is passionate about how research can improve care.
He said: “It takes a long time for clinical evidence to work its way into routine practice. Covid is an example of rapid evidence into practice through vaccination, however for example patients who present with acute strokes may not yet be receiving the best treatment based on where they live or the day of the week.
“Minimising the delay can benefit many and improve chances of a better recovery. We see a similar example in the fact that it took many years for all hospitals to adopt NEWS and create a common language for all health care staff to assess how sick a patient is.
“This will involve designing systems to make it routine in hospitals. Hospital and system design is important for patients and staff to ensure the right care, right time, first time – this ranges from the physical design of a building to the optimal use of IT.
“This work has involved visits to several countries abroad including Australia, Singapore, Pakistan, Bangladesh and Nepal.
“It also means having enough staff to carry it out and we need to train more staff in acute and general medicine because we can do an increasing amount for patients, and we know what to do.”
He has retired from the wards but is chair of two hospital trusts in North Tees and Hartlepool, and South Tees and says his faith in the NHS is undimmed.
“Treatment has to remain free for our children, grandchildren and beyond, and patients must get the best available,” he said. “The NHS has changed hugely since I started working for it in 1980 and will continue to do so as it remains superb institution.”
It is nice to get a minute’s clap but most nurses want safer wards
– Vanessa Martin
by Sally McDonald
Businessman Brian Salmon shaped Britain’s culinary culture when he introduced the Wimpy hamburger to Britain but to Vanessa Martin, one of Scotland’s most experienced nurses, he had a far more influential – and detrimental – role on the National Health Service.
In 1967, he led an investigation into how nurses should be integrated into NHS management structures and, according to Martin, one of Scotland’s most experienced nurses, the changes recommended by the Salmon Report would have far-reaching and hugely-damaging consequences for the NHS as senior nurses were encouraged into management roles and away from the frontline of patient care.
She believes making administrative roles the best-paid jobs for ambitious nurses prompted a catastrophic and enduring drain of talent from the wards after the Salmon Report’s recommendations were implemented in 1973.
Martin, 77, who spent most of her career on paediatric and surgical wards and was a nursing sister and the Royal College of Nursing’s Nurse of the Year in 2000, said: “It was one of the lows of my career. It put nurses into grades across the UK with a management structure that we didn’t have before. In the health service now, there are very few senior nurses on the frontline.”
The recommendations meant the lowest salary grade – band five – was set for newly qualified staff, rising to a band seven. Those in bands eight to 10 became purely management.
Today the starting pay for band five nurses in the NHS is £26,104.
Martin claimed: “Most of the staff nurses you find on wards today are a band five. That’s because of the NHS trying to save money. You might find the occasional band six, or a band five nurse with 10 years’ experience, but band sevens are practically extinct now in Scotland.
“I was a band seven supervisory, supernumerary ward sister and, because I did not have a caseload I was free to oversee the ward. My role was to go on the rounds to make sure every care was implemented for every patient. I was also responsible for overseeing the teaching of the students on the ward.”
Eventually, she was required to pick up a caseload and was downgraded to band six which she claimed meant her ability to supervise and train was lost.
Today, looking back on the changes she has seen in the NHS and at the current worrying staffing levels, she believes it is time to take the focus from management roles and place it on frontline care.
Martin – who was latterly the clinical director of a cleft lip and palate service for East Midlands and worked with a Westminster government steering committee setting standards and monitoring its national re-organisation of the service – has a radical vision for the NHS.
She said: “I want to go back to the structure we had before Salmon with more senior staff nurses on the wards lead by a supervisory sister.”
While she welcomed the introduction of university degree training for nurses and the creation of specialist nurses in specific fields, she said she would also like to see within the NHS a new branch of nursing dedicated purely to care of the elderly and their specific medical issues.
She believes this would relieve stress elsewhere in the service, and put an end to the “phenomenal costs” of private nursing homes, while at the same time boosting training, development and retention of quality NHS staff.
Martin remembers like yesterday the moment she donned her first uniform; dress hem a regulation 15 inches from the ground, hair strictly above her starched white collar and caught neatly in white cap.
Much has changed since the Gatehouse of Fleet grandmother started her training in 1962 at London’s world-renowned Great Ormond Street Children’s Hospital where matron reigned supreme.
But as she prepares for the launch of her memoir, The Great Ormond Street Nurse, the secretary of the RCN’s Dumfries & Galloway branch said the impact of Covid was leading to “a tsunami” of mental health and stress-related problems and post traumatic stress among staff.
This, she fears, is compounded by pre-existing and worsening nurse shortages with junior nurses often bearing the brunt of patient care. Now she fears the exodus of staff will compromise patient safety.
She said: “The under-staffing in hospitals now is a real problem, particularly with senior nursing staff across Scotland. Our registration body, the Nursing and Midwifery Council, operates for the whole of the UK, including Scotland, Wales and Northern Ireland.
“Last month it reported that some 13,945 nurses, midwives and nursing associates left the register between April 1 and September 30, 2021 – a four-year high. These people have actually cancelled their registration with the NMC, so they have left nursing entirely.
“People are constantly saying, ‘it is very nice to be clapped [by the public during lockdown] but we would rather have more salary and safer staffing. Safer staffing is the biggest thing.
“During my career as the supervisory sister, I would have at least three or maybe four senior staff nurses, about four junior staff nurses, state enrolled nurses, and at least two unqualified staff. Now the wards are run mostly by junior staff nurses.”
She said there were more unqualified staff on the wards today than in her time. And she claimed: “I have heard reports of qualified nurses being responsible for 14 patients each; that’s not safe.”
The only set staff-to-patient ratio currently recommended in Scotland is in adult high dependency where there should be one registered nurse for every patient (or one registered nurse to two patients in critical care settings).
In all other services, safe staffing levels are dependent on the type of care being given and the dependency of patients, and other factors.
Although the RCN hasn’t recommended staff-to-patient ratios for other services, it has repeatedly pointed out registered nurse numbers are vital to ensuring safe care and has called for the implementation of legislation passed in the Health and Care (Staffing) (Scotland) Act 2019 to help ensure safe staff levels in hospitals and care homes.
Martin said: “What has changed most over the decades since I was training and is the biggest issue is staffing. It’s a huge problem and it’s because pay is so low.”
In May 2021 – the same month Nicola Sturgeon announced a 4% salary hike for nurses – the RCN claimed the pay of an experienced nurse had fallen by 15.3% in real terms over the past 10 years. It had called for a 12% raise.
Martin said: “That is a huge drop.”
Issues with continuing professional development, like financial restraints and lack of cover for the staff involved, also contributed to decisions to quit, she said.
And the pandemic had brought matters to tipping point. She said: “Covid-19 has been very distressing for staff because of the hours they work and the huge pressures they have been under. There is a certain amount of post traumatic stress disorder in nurses. The RCN is providing services to support them.
“When the first lock down was lifted, we had mental health nurses saying it was like a tsunami and that they didn’t know where to turn with the mental health problems coming through. One of the staff who was in the Army happened to mention that she felt that in the Falklands – which was traumatic in the extreme – she was better supported by the Army than the NHS.”
The Great Ormond Street Nurse: The life of a trainee nurse at GOSH in the 1960s, by Vanessa Martin, is published by Wellbeck on Thursday

Enjoy the convenience of having The Sunday Post delivered as a digital ePaper straight to your smartphone, tablet or computer.
Subscribe for only £5.49 a month and enjoy all the benefits of the printed paper as a digital replica.
Subscribe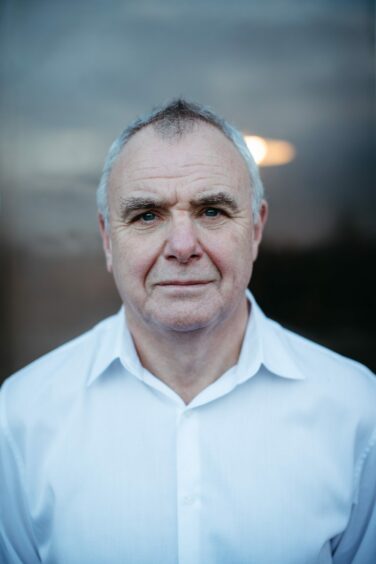 © Andrew Cawley
© Andrew Cawley © Andrew Cawley
© Andrew Cawley
 © Jamie Williamson
© Jamie Williamson © SYSTEM
© SYSTEM